Lifting Buddy - The Left Ventricular Assist Device
- foamfrat
- Dec 31, 2024
- 6 min read

Anyone who has tried a little resistance training knows that a lifting buddy can help lighten the load and ensure you have enough strength to prevent yourself from getting smothered by the bar. They may have to pick up the slack even more on days you are feeling weak, but a good lifting buddy helps you build strength and improve performance. The LVAD is a device for the weak heart that still requires some cardiac effort, but takes some the majority of burden off the LV.
We will not frequently encounter one of these in the field, but if you aren't prepared, it can be a little intimidating. Let's start with a:
Quick Terminology Refresher
Mechanical Circulatory Support Device (MCS): General term for any device that aids the heart, whether temporarily or permanently.
Ventricular Assist Device (VAD): This device specifically supports the ventricles; it can be left, right, or both.
Controller: The device that manages the pump
Total Artificial Heart (TAH): Replaces both lower ventricles with mechanical devices
The Devices
There are various models that essentially do the same thing. Standard devices include the HEARTMATE II, HEARTMATE 3, HEARTWARE HVAD, JARVIK 2000, and Total Artificial Heart FreedomTM Driver System. The benefit is that pre-hospital patients have the same treatment plans.

The LVAD assists the left ventricle in pumping blood, not replacing it. This improves patients' quality of life by alleviating heart failure symptoms.
Additionally, you do not have to be a candidate for a heart transplant to receive an LVAD; this is a common myth. There are essentially two categories of patients: Bridge to heart transplant and Bridge to destination. The destination is an improved quality of life.
This does not mean they are running marathons - the patient’s life will revolve around this LVAD.
Want to see a movie? I hope my heart batteries are charged.
Want to visit the grandchildren? I hope I can get back to my heart doctor should something happen.
Despite some of the logistical nuances of an LVAD, Mobility considerably improves their quality of life. Generally, these patients would sit at home, sleep in their recliner, and then get short of breath just thinking about getting up and using the restroom (Cabrera, 2014).

Vitals
With most LVADS, you will not have a palpable pulse point. So does this mean we cannot obtain a blood pressure?
Is The LVAD Functioning?
We can listen to the patient's chest for a humming or buzzing sound. This tells us that there is some blood flow through the body. One fortunate aspect of these devices is that a patient can maintain ventricular tachycardia or ventricular fibrillation much better than the average person. The reason is that the pump continuously (slight) flows blood. This occurs independently of what is happening electrically in the heart (Mechanical Circulatory Support, 2020).

Pulse:
It is often not palpable. Blood flow can be monitored through a Doppler device or by auscultating a "humming" sound.
Blood Pressure:
Measured through Mean Arterial Pressure (MAP) using electronic monitors or Doppler devices. A MAP around 70-90 mmHg is typical. Remember that the healthier the native function, the more likely your automatic will be accurate.

Other Indicators:
EtCO2 Monitoring, Skin Condition, Temperature, Mentation, Cap refill
One benefit to most providers is that we generally use electronic monitors that take automatic blood pressure. These monitors measure mean arterial pressure (MAP) and then extrapolate systolic and diastolic based on a proprietary algorithm that determines how far to the right and left of the highest oscillation the sys/dia will be located.
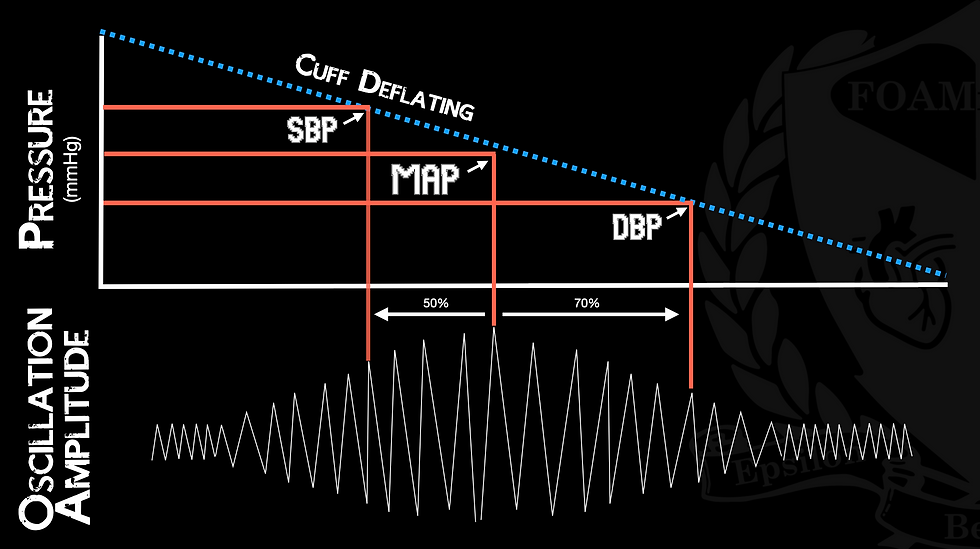
It is relatively common for LVAD patients to be issued a personal doppler. This is because the gradient between systole and diastole is so close, they essentially become the same. Therefore, the mean pressure within the arterial tree is heard as the first "swoosh" on the Doppler as we release the pressure from the cuff. The clinician would inflate the blood pressure cuff and use the Doppler as with a stethoscope.
Treatment
Looking at actual treatment modalities. Essentially, to put this blog to rest… You will treat the patient the same as any other patient. Please do not get task-saturated as soon as you see they have an LVAD. Should the patient have an arrhythmia, manage the arrhythmia as you were trained to do. Per the manufacturer's recommendations, these devices are safe to use with all medications, external pacing, and cardioversion. However, as we talk about treatments here, there are a couple of takeaways.
Call the LVAD coordinator.
Take ALL of their LVAD equipment with you to the hospital
Batteries, Spare batteries, Wall Plug Adapter, Cords, Plugs, and Patience
REGARDLESS of their complaint, these patients must be transported to an “LVAD Competent Facility” (VAD, n.d.). Preferably where they had their LVAD put in; however, you are not going to fly GramGram back to Nebraska when she is visiting family in Rhode Island.
These patients are complex… for the hospital. 99% of the time, they have statistically few problems. With that being said, the manufacturers say that CPR, medications, Defibrillation, Cardioversion, and Anything you would normally do are OKAY. However, I empower you to use this as a starting place. These patients will have an LVAD Coordinator, the Poison Control of LVADs. These people can direct resuscitation efforts based on the information you provide them (i.e., alarms, vitals, rhythms).
CPR?
The age-old question of CPR… it depends. Manufacturer recommendations and several other PubMed articles state it is okay to perform CPR. However, this will rely heavily on policy, procedure, and protocol. Additionally, contact the LVAD coordinator, and they can help guide resuscitation efforts. However, all the same medications and algorithms work here. We still defibrillate ventricular fibrillation just as we would any other patient. The odd thing here, though, is that these patients generally tolerate arrhythmias much better. For example, a patient with Ventricular Tachycardia may be awake, alert, and oriented for an extensive period. The LVAD continues to push blood through without caring for the electrical activity. Therefore, take a breath and calm down. After reading this awesome paper, we should feel more at ease treating these patients (PMID: 30202496; AHA (Peberdy et al., 2017); PMID: 31914051).
Problems
Hypovolemia
If you are going through a simulated LVAD scenario, it is almost guaranteed that the patient will be hypovolemic, and there is absolutely nothing wrong with the pump. LVADs are preload-dependent devices (kind of like the heart, but more). If the patient is dry or if something is obstructing venous return, there is nothing to pump out of the LV. Always make sure you think about volume status before assuming the LVAD is broken.
Bleeding Risk
Due to the blood taking a ride through a mechanical pump, these patients will be on anticoagulants. Just like any other patient on anticoagulants, complications can include GI bleeds, head bleeds, etc.
Pump Thrombosis
You will probably not even know the patient has a pump thrombosis. These often present with generalized malaise and an intermittent “low flow alarm.” The low flow is caused by a clot clogging the LVAD. However, this is all the more evidence to confirm these patients need to be transported to an LVAD-competent facility. These patients will generally be on a blood thinner (usually Coumadin); however, they may also be on aspirin. This inherently helps them with the thrombosis problem. The body does not love anything foreign inside of itself, when it detects this, we always have the possibility of clot formation (Trinquero, 2018).
Key Takeaways
Communication: Always involve the LVAD coordinator for guidance on specific situations.
Patient Handling: Despite the complexity of LVADs, remember to treat the patient with the same care and principles you would apply to any other patient in an emergency.
Transportation: Prioritize transporting to an LVAD-competent facility when possible.
By understanding and preparing for the unique needs of LVAD patients, we can improve outcomes and provide better care.
Christian T. Meyer
Also, checkout https://www.mylvad.com/medical-professionals/resource-library/ems-field-guides for a great EMS resource on the various devices.
References
Cabrera, Daniel. (Nov 2, 2014). A Basic Approach to the LVAD Patient in the Emergency
Department.
https://emblog.mayo.edu/2014/11/02/a-basic-approach-to-the-lvad-patient-in-the-emergency-department/
Choi, H, & Merrill, S. (2023). EMS Left Ventricular Assist Device Management. In StatPearls.
StatPearls Publishing. PMID: 30252243
DeMers, D & Wachs, D. (Apr 10, 2023). Physiology, Mean Arterial Pressure. In: StatPearls.
Homan, T; Bordes, S; Cichowski, E. (Jul 10, 2023). Physiology, Pulse Pressure. In: StatPearls.
Iwashita, Y; Ito, A; Sasaki, K; Suzuki, K; Fujioka, M; Maruyama, K; Imai, H. (2020).
Cardiopulmonary Resuscitation of a Cardiac Arrest Patient With Left Ventricular Assist Device In An Out-Of-Hospital Setting: A Case Report. Medicine, 99(2), e18658. https://doi.org/10.1097/MD.0000000000018658
Mechanical Circulatory Support Emergency Guide 2020-2021. (2020). International Consortium
Of Circulatory Assist Clinicians. https://www.mylvad.com/sites/default/files/EMS%20Field%20Guides/2021%20Field%20Guides/ICCAC_Emergency_Guides_20_21-1.pdf
Peberdy, M; , Gluck, A; Ornato, P; Bermudez, A; Griffin, E; Kasirajan, V; Kerber, E; Lewis, F;
Link, S; Miller, C; Teuteberg, J; Thiagarajan, R; Weiss, M; O’Neil, B. (2017). Cardiopulmonary Resuscitation in Adults and Children With Mechanical Circulatory Support: A Scientific Statement From the American Heart Association. Circulation, 135(24). https://doi.org/10.1161/cir.0000000000000504
Tchantchaleishvili, V; Sagebin, F; Ross, R. E; Hallinan, W; Schwarz, K; Massey,T. (2014).
Evaluation And Treatment Of Pump Thrombosis and Hemolysis. Annals of Cardiothoracic Surgery, 3(5), 490–495. https://doi.org/10.3978/j.issn.2225-319X.2014.09.01
Trinquero, P; Pirotte, A; Gallagher, L; Iwaki, K; Beach, C; Wilcox, E. (2018). Left Ventricular
Assist Device Management in the Emergency Department. The Western Journal of Emergency Medicine, 19(5), 834–841. https://doi.org/10.5811/westjem.2018.5.37023
Ventricular Assist Devices (VAD) | CMS. (n.d.). Www.cms.gov.




