
I am not sure why I have been so obsessed with obstructive vent strategies lately. We understand the concept of prolonging the exhalation phase, but do we understand when this is necessary? How to identify occult PEEP? And how simple adjustments make significant changes?
I decided that in order to reinforce these concepts into our providers minds, as well as my own, it would require me building a device in which you could simulate obstructive airflow in both the asthmatic and emphysematous patient. This would beget an understanding of how each obstructive process differs in its mechanism that causes restricted expiratory airflow.
The Experiment
I started off with my vent circuit and test lung. I would need to create a narrow caliber attachment to connect the distal end of the circuit to my test lung. I decided to use an 8.5 ETT with the shell of a pen inside. Both ends of the tube would be fitted with a 15mm adapter in order to connect to the circuit and test lung.
Caliber Reduction
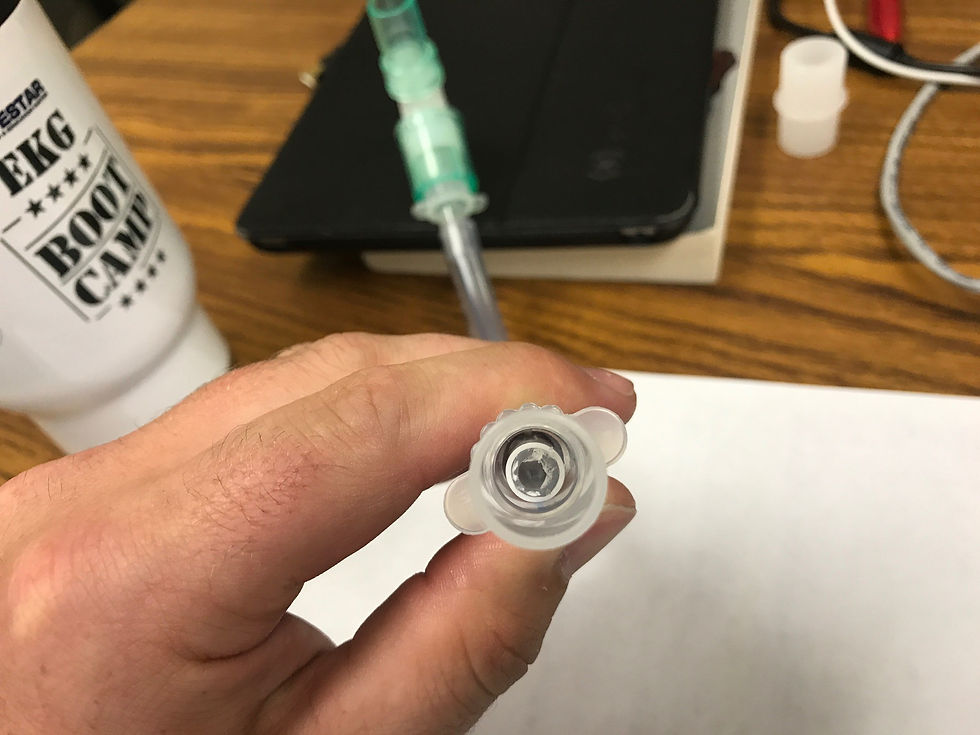
Interestingly, the airflow restriction that this created was not quite enough to generate auto PEEP unless I increased the frequency or Vt. In order to make this more realistic, I used a 1cc syringe with the flange cut off. This fit nicely in the shell of the pen. What's nice about this fit is the ability for the syringe to slide through the barrel of the pen on inhalation, yet obstruct the airway during exhalation. This simulates an emphysema patient who is able to get air in, however causes obstruction when the diseased elastin collapses during exhalation.

If you want to avoid the ease of inspiratory flow, and create a consistent narrowing of the airway caliber, you can fix the syringe tightly in the pen. This will eliminate the "one way valve" movement. This is a great way to simulate an asthmatic patient. Commonly we hear "asthmatics have a harder time getting the air out rather than in." This is generally the case in the beginning of asthma due to the increase muscular recruitment that is utilized to create the active phase of inhalation. As we all know, this will eventually diminish as the patient becomes fatigued.
Hidden PEEP!
What I found most interesting about this experiment, is that the Auto PEEP is underestimated on the pressure waveform unless you employ an "E Hold" maneuver. This is due to the fact that dynamic auto PEEP reflects the lowest regional auto PEEP and subsequently underestimates static auto PEEP. Maltias et al (1) demonstrated that accumulative auto PEEP is best detected utilizing a static measurement in a patient is who not spontaneously breathing. Factors that may contribute to the peripheral airways not communicating with proximal airways are mucous hypersecretion or increased wall thickness(2).

This simulator will demonstrate to students that even though you are clearly air trapping, the ventilator will not always detect the occult PEEP. This is shown in the video below.
Reading about this phenomenon is beneficial, but being able to simulate this in front of a group of students has been a goal of mine. This project will continue to develop and be revised. This is the first step in the right direction!
I am sure there will be many modifications and improvements to this concept. Please share your experiments with us by pinging @FOAMfrat on Twitter!
1.Maltais F, Reissmann H, Navalesi P,et al. Comparison of static and dynamic measurements of intrinsic PEEP in mechanically ventilated patients with severe asthma. Crit Care Med 1996; 24:541-546.
2.Rossi A, Gottfried SB, Zocchi L, et al. Measurement of static compliance of the total respiratory system in patients with acute respiratory failure during mechanical ventilation. The effect of intrinsic positive end-expiratory pressure. Am rev respire Dis 131:672-677.
